What is Immunotherapy?
Every moment of every day, our immune system asks the same question, over and over: Is this me?
The cells of your immune system are the security forces that patrol the borders, towns, and streets of your body, seeking harmful invaders.
There are the obvious border incursions, such as when harmful bacteria enter through cuts in your skin. These are handled by the neutrophils, monocytes, and ‘natural killer cells’ of your innate immune system.
Then there are the ‘special agents’ of your adaptive immune system – lymphocytes called T-cells and B-cells – which seek out those invaders that by stealth and subterfuge have made it deep into your body’s interior. These lymphocytes need to be trained to differentiate between your own cells and an infection.
This training is highly specialised and effective:
each T-cell or B-cell recognises and reacts to only one of the tens of
thousands of substances – called antigens – that can trigger an immune
response.
Many millions of years of evolution have given your immune system the capacity to recognise a plethora of bacteria, viruses, and fungal spores that have the potential to make you seriously ill.
“The immune system has got to be really clever,” says Professor David Gottlieb of the Westmead Institute for Medical Research in Sydney.
Why do things go wrong?
We only have a very small number of each highly specialised type of lymphocyte in our body. It’s impossible for us to constantly maintain large numbers of antigen-specific T-cells and B-cells, given the multitude of antigens that we may be exposed to.
This means it can take several days for our immune system to mount a sufficient response once an infection is detected, and by this time, we can already be very ill. This is especially so for young children whose adaptive immune system is still being ‘trained’.
If you’re familiar with immunotherapy, you’ll know that it describes any intervention that manipulates the immune system for therapeutic benefit. The vast majority of us have undergone the most common form of this – immunisation via vaccines – as kids.
Vaccines trigger the production of immune cells by imitating an infection with a weakened or inactive form of a virus or bacterium.
Much of the focus – and excitement – of current clinical research is around the potential to use new forms of immunotherapy to cure traditionally untreatable cancers. Because our immune system might be shrewd, but so are cancer cells.
Patrolling T-cells can receive an ‘at ease’ command from other cells they meet so they don’t become too aggressive. This is known as a ‘checkpoint’, and it works when a checkpoint protein on the surface of the T-cell is triggered by a matching protein on the cell that it’s interrogating. In this instance, the T-cell is told to stand down.
The matching protein acts like the cell’s identity papers: it signals to the T-cell that this cell isn’t foreign or defective and has a right to be there. Effectively, the cell is saying to the T-cell, “Don’t attack me.”
But cancer cells also sometimes carry this matching protein – a set of fake identity papers that fools the T-cells into letting them continue on unchallenged.
Recent advances in immunotherapy are allowing clinicians to biochemically override these identity checks to unleash a massive attack of T-cells on tumours. The most common form of immunotherapy is called checkpoint inhibition therapy.
Checkpoint inhibition therapy
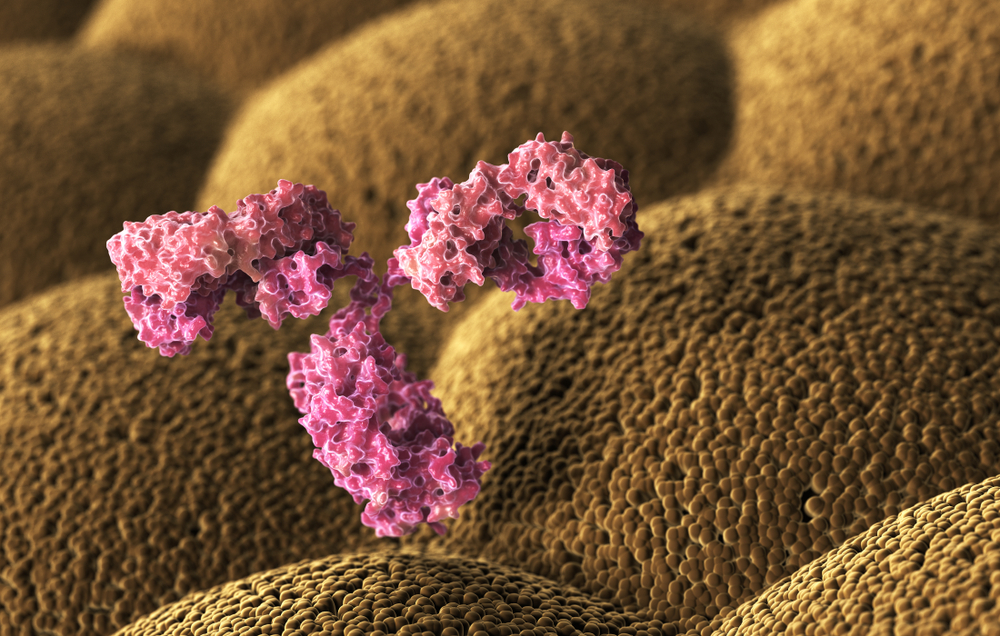
Checkpoint inhibitors are antibodies that block the interaction between a T-cell’s ‘at ease’ receptor and other cells’ identity proteins.
When clinicians administer checkpoint inhibitors to a patient, they are blocking the “This is me!” message to the T-cells. This causes the T-cells to become indiscriminate killers of friend and foe cells alike.
It’s like a general giving the order “Charge!” to his army, says Gottlieb: “Go and find things and kill them.”
Checkpoint inhibitors have high response rates in cancers such as melanoma and Hodgkin’s lymphoma. Researchers believe this is because these cancers have, on average, more genetic mutations, and therefore more antigens, than some other cancers.
Each new antigen attracts an immune system response, especially when all of your body’s T-cells have been ordered to attack.
One of the consequences of allowing this indiscriminate attack by the T-cells is significant rates of autoimmune disease, which accompanies checkpoint inhibition therapy, says Gottlieb. This is when the indiscriminate attack lets T-cells kill everything, including normal cells. It’s the equivalent of being killed by friendly fire.
For melanoma treatment, this can range from relatively harmless diseases such as vitiligo, where T-cells attack melanin-producing skin cells causing skin discolouration, to serious conditions such as ulcerative colitis, an inflammatory bowel disease.
The future is now
Where immunotherapy meets precision medicine – a recent move towards more personalised, targeted treatment – we get what’s known as adoptive T-cell therapy. This holds the promise of harnessing our body’s own T-cells to more accurately target the treatment of cancer and infectious diseases.
There are more than one type:
1. Infection- and tumour-specific T-cell therapy takes a small number of highly specific T-cells that normally exist in our body, stimulates them in the laboratory to grow to large numbers, and then infuses them in their billions back into the blood stream
It’s a simple idea, but this new approach can be adopted to treat many different types of viruses for which there are no effective treatments. The cells already exist, but just need encouragement to grow to large numbers.
Infection-specific T-cell therapy is a promising treatment for drug-resistant infections in patients whose immune system has been strongly suppressed, such as people undergoing chemotherapy, or organ or stem cell transplants. Very few side effects have been noted.
Research on adoptive therapy using tumour-infiltrating lymphocytes to treat cancer is less advanced, but has shown some effectiveness in treating metastatic melanoma.
2. CAR T-cell therapy is where the big excitement in immunotherapy is right now. CAR T-cells don’t normally exist in the body. Instead, scientists insert an entirely new gene into T-cells from a patient’s blood. This gene is expressed as a synthetic protein, called a chimeric antigen receptor (CAR).
The resultant ‘CAR T-cells’ are then grown in the lab and infused back into the patient’s bloodstream. The synthetic receptor on the CAR T-cell is designed to bind to a specific protein on cancer cells.
It’s akin to your T-cells becoming the Bionic Man – still human, but technologically enhanced to recognise cancer cells by their features. CAR T-cells can seek out and kill cancer cells with great precision.
These T-cells are so active that, although they might get a signal from the ‘identity protein’ on cancer cells to stand down, they still kill the cells anyway.
CAR T-cell therapy has a high response rate in some forms of acute leukaemia and a good response rate in some forms of lymphoma – both cancers of the blood.
Like any living cell, CAR T-cells have the ability to divide and grow inside our bodies. When CAR T-cells are infused into a patient with a high cancer load, they become “totally switched on”, says Gottlieb.
Totally switched-on T-cells release a lot of cytokine – a protein that causes inflammation. This can lead to cytokine release syndrome which, in some patients, causes a potentially lethal inflammatory response.
Will immunotherapy be the cure for cancer?
“There isn’t a single cure for cancer,” says Gottlieb. “There are advances in particular cancers, and immunotherapy seems to be a really significant one for some very common cancer types.”
The modern forms of immunotherapy are curing some cancers that would otherwise not be curable. In some cases, it’s occurring in a significant proportion of patients who would otherwise have no hope, says Gottlieb.
But checkpoint inhibition and CAR T-cell therapy have not yet proven effective for the most common cancers, such as breast, colon, prostate, and lung cancer, and Gottlieb stresses that both are still at a very early stage of development.
“That’s the next frontier really, trying to get the sorts of immunotherapies that have proven to be a revelation in some types of leukaemia and lymphoma, and trying to work out how to apply them to the really common types of cancers,” he says.
The next wave of immunotherapy trials will be combining different types of immunotherapy, and using them alongside some of the less toxic chemotherapy drugs.
With luck, the harmful side effects will be reduced, and the control of diseases will be improved.
“That’s all to be discovered,” says Gottlieb.
By Viki Cramer
Updated 4 months ago