Solving a heart problem with tools from the oil industry
In cardiac care, replacing the mitral valve is a conundrum. While new surgical techniques are now making it easier and less invasive to replace a damaged aortic valve, applying those same techniques to the mitral valve is more complicated.
Dr James Otton wants to crack the problem by applying sophisticated 3D modelling and software tools more at home in the aeronautics and oil industries. For patients – older patients especially – it could be a lifesaver, sparing them open-heart surgery.
So far, results are promising and Otton has been awarded a NSW Health Cardiovascular Early-Mid Career Researcher Grant to support gathering more data on the game-changing potential of computer simulation.
Otton combined study in arts and medicine at the University of New South Wales (UNSW) before settling on a career in cardiology. “It combines physiology and understanding,” he reflects. “A lot of the time we can fix people’s problems with medication or procedures. And like many people in Australia, I have had people in my family suffer from serious heart issues. My dad died with heart disease when I was 16 and that’s also a motivating factor.”
Sydney-based Otton runs a cardio-oncology clinic at his base at Liverpool Hospital, consults at St Vincent’s Private and is affiliated with UNSW. He first encountered the mitral valve problem when working with colleague Professor David Muller, a pioneer in valve replacement procedure at St Vincent’s Hospital in Sydney. With a background in biomedical engineering, Otton thought imaging and computer simulation might provide a solution.
Heart valve replacement, until recently, meant opening the chest, stopping the heart, placing the patient on a heart-lung machine, cutting out the old valve and stitching in a new one. While it’s a relatively routine procedure, the need for a prolonged ICU stay and a long recovery period is particularly taxing for elderly and very sick patients.
Transcatheter valve replacement however, has changed the landscape in the last decade. A small cut at the top of the leg admits a catheter to carry a new valve to where it is needed. The valve is expanded and the patient has a new aortic or mitral valve without the need for open-heart surgery.
“Just last week I had a 97-year-old patient who still lives at home and is pretty independent, she had one of these procedures,” Otton says. “It means she won’t have to go to a nursing home, and she has a good quality of life.”
What’s good for the aortic valve however, is not always good for the mitral valve, which controls blood flow through the left atrium and ventricle. The valve can be damaged in a range of ways – from congenital conditions to infection or heart attack. And, it degrades with age: most patients needing mitral valve replacement are older.
The shape and location of the mitral valve mean positioning the new valve can be problematic; it can actually block blood flow out of the heart and this obvious danger means not every patient is a suitable candidate.
“We’ve been trying to work out who can have these valves and who can’t, who might have a complication,” Otton explains. “We’ve been using pretty simply measures – drawing areas, trying to work out how the valve will sit, but the heart’s a moving structure, it’s very complicated. I realised we could use much more sophisticated methods of computer simulation to solve this clinical problem.”
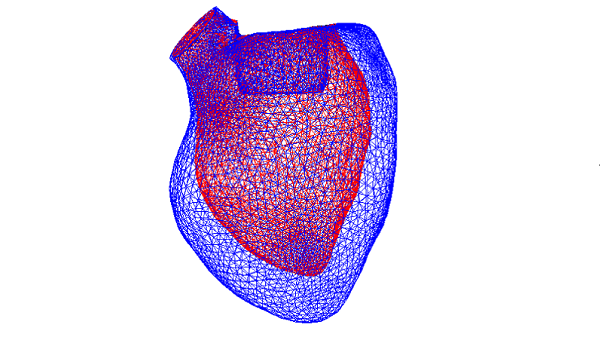
Advanced CT imaging is key. Otton’s team creates very detailed 3D images of the moving heart to which they apply a fluid simulation software tool commonly used in the aeronautics and oil industries.
“We take a 3D model of the valve, we simulate where we’re going to put that valve and we run the simulation for that person’s anatomy, for their heart valve position. We work out how the blood is going to leave the heart and we can predict if there’s going to be a problem,” he explains. Positioning of the valve can be adjusted and, often, the problem overcome.
The NSW Health grant will assist Otton, working out of the School of Biomedical Engineering at UNSW, to run existing cases through simulation and compare them with final results. It will also help him simplify the process.
“Cardiologists are not going to run computational flow dynamic computer programs, so we also need to make this computer simulation process very quick and easy, to help people decide on these procedures in real time.”
The NSW Health Cardiovascular Early-Mid Career Researcher Grant presents an exciting opportunity to innovate, Otton says. He’s also benefitted from NSW Health’s other innovative initiatives, like the Medical Device Commercialisation Training Program, which focuses on the commercialisation of bright ideas like his.
It’s early days, but he’s hoping transcatheter mitral valve replacements will eventually be feasible for 80 to 90% of candidates considered for the procedure.
“I can remember when elderly mitral valve patients would not have anything available to them. I’ve also seen people struggle to recover from heart surgery, so these transcatheter valves, as a clinician, really do excite me and bring my patients immediate benefits. We’re hoping to do that for more people in the future.”
Updated 5 years ago