NSW Government research grant helps boost genome sequencing techniques to track COVID-19
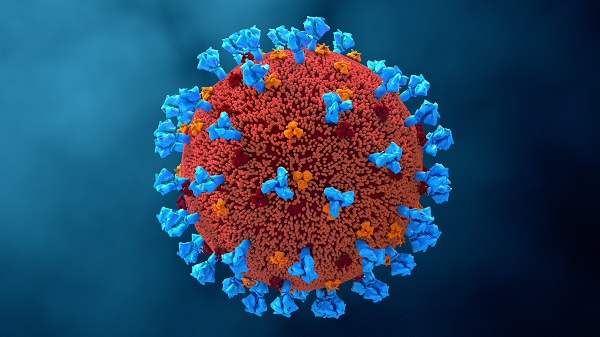
Whole genome sequencing rarely results in breaking news alerts, but the COVID-19 crisis has put science squarely on page one. Few stories in the daily news cycle are more compelling than those about transmission chains of the coronavirus.
Sequencing the genome of the virus culprit during a global pandemic enables health professionals to track, trace and stop the disease. Many hundreds of cases have been sequenced in Australia, revealing links between infections and supporting the response teams to prevent ongoing transmission. But patients at different stages of this disease can have different amounts of virus present: too little virus and samples can be difficult to sequence, threatening to derail this detective work by causing critical links between cases to slip under the radar.
Professor Vitali Sintchenko and a team of infectious disease experts from the University of Sydney and NSW Health Pathology have been awarded a NSW Health COVID-19 Research Grant to explore ways to plug this gap in genomic surveillance. It will help fund translational research into new testing methods that are expected to boost the numbers of samples that can be successfully sequenced.
The stakes couldn’t be higher, nor the responsibility greater. Working in tandem with epidemiologists, who ask questions of people within the community and trace contacts to understand and control disease spread, scientists like Sintchenko and his collaborators contribute to crucial policy decisions.
“We save time for the epidemiologists,” he explains. “They have the level of confidence to go to the government and say, well, it’s very likely — as likely as it can be — that this is a sample from Victoria or from the USA, or it’s not a sample from Victoria or USA. Or, this is a hospital associated infection, or likely to be a transmission from a health care facility. To make that claim, knowing it will be in the newspapers, it may be challenged and questioned by lawyers, you need this information.”
Quality information is key. As Director of the Centre for Infectious Diseases and Microbiology – Public Health in NSW, Sintchenko and his colleagues have been honing genotyping techniques for over a decade, but the advent of portable bench-type sequencing machines meant that technology once accessible only at Harvard and Cambridge became available in Sydney in 2015. Funding from NSW Health’s Office for Health and Medical Research soon provided next-generation sequencing equipment and with it, capacity to explore diseases of public health concern such as TB and salmonella, building capability vital to Australia’s pandemic response.
Sintchenko and his team sequenced the genome responsible for the first case of COVID-19 in NSW in January and have sequenced more than 600 since, revealing and reporting clusters and transmission links to NSW Health COVID-19 tracers. But the need for greater sensitivity in testing has emerged as a pressure point.
The challenge of whole genome sequencing is that it requires at least 80% of the genome to be present in order to be effective for transmission tracking. A poor sample — perhaps from a too-gentle respiratory swab or an asymptomatic patient carrying a small amount of virus — could be the difference between identifying a known line of transmission or missing a case in the community that needs urgent tracing to halt the spread.
The new methods the collaborative research team is investigating rely on innovative ways to concentrate the target virus in low-yield samples and fish out longer portions of coronavirus genomes from them.
So far, they have completed three ‘runs’ using their new procedure, but will need to do 100 more to be certain of its efficacy, which is where the research grant can be put to immediate use.
“Then we will replace our current method with this new, more powerful, more sensitive and more appropriate method,” Sintchenko says. “That’s the gist of the project. We plan to examine this with retrospective samples first and then test it in our laboratory in real life and then, within 12 months, implement this method as a routine.”
“This information gives public health officials and clinicians important evidence from science to build these responses in a timely fashion and to be more comfortable in their decision-making.”
By Michelle Schlechta
Updated 5 years ago