Melanoma breakthroughs
Through world-leading genetic work, NSW researchers are discovering why about 50% of melanomas don’t respond to immunotherapy.
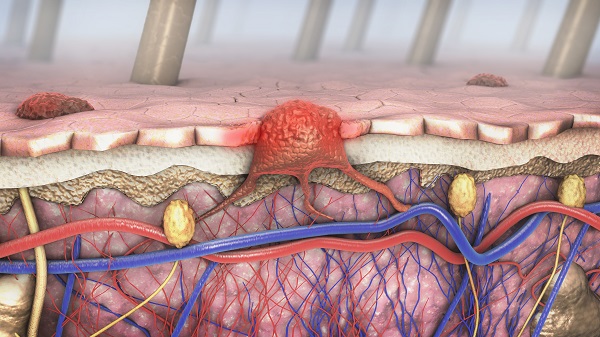
Over the past decade, immunotherapy drugs have become the standard treatment for metastatic (or Stage IV) melanomas. These drugs help someone’s immune system recognise and fight a tumour by preventing tumour cells from obstructing the body’s immune checkpoints. Unfortunately, in half the patients, these drugs don’t work.
‘About 50% of patients achieve a long-term benefit from these drugs, so we want to identify them quickly,’ says Dr James Wilmott, research leader of the Translational Melanoma Research Group of the Melanoma Institute Australia at The University of Sydney. ‘But of those who don’t respond, up to 43% have severe toxicity as a result of the treatment – the drugs might actually make them sicker.’
Dr Wilmott is part of a research group that is endeavouring to understand the genetic reasons behind why some melanomas don’t respond to immune checkpoint inhibitors, and whether there are treatments that will work. Since 2015, five papers have been published on this world-leading work, much of which stemmed from a grant from the Sydney Genomics Collaborative. The grant enabled whole genome sequencing of 91 patients with metastatic melanoma who had either responded, or not responded, to immunotherapies. Whole genome sequencing – looking at all the genetic material of a patient rather than just the protein coding regions – has now been completed on more than 500 people with melanoma, making it the largest study of its kind in the world.
Dr Wilmott says the studies have shown that melanomas respond in different ways to treatment, depending on the cause and location of the melanoma, with genetic mutations highly related to where the melanoma originates.
Cutaneous melanomas, which occur in sun-damaged skin, are more likely to respond to immunotherapies than uveal, mucosal or acral melanomas. (Uveal melanomas are those in the eye, mucosal in areas such as the ano-genital and urinary tract, and acral melanomas – which are very common in dark-skinned people such as those with African and Asian heritage – are found under the fingernails or on the soles of the feet.) This is partly because most sun-caused melanomas have many genetic mutations.
‘If you have more mutations, the chance of your body recognising there’s something wrong goes up,’ he says. ‘Some of the patients have over a million mutations in their DNA. But in mucosal melanomas you get a lot fewer mutations – as little as 14.’
The team discovered that the melanomas that don’t respond to treatment are very different genetically, with a wide range of different mutations causing the melanomas. Many of these mutations have previously not been documented in these melanomas. ‘We’ve been discovering that the patients who are not responding to immunotherapy are all very different,’ Dr Wilmott says. ‘So we’re starting clinical trials to test if we can get better results with immunotherapy, by giving each individual patient a drug based on their own tumour.’
For example, although most of the mucosal melanomas had a low level of mutations, making them less likely to respond to treatment, a small number had a very large number of mutations, so they might respond.
Whereas some clinical researchers around the world keep their data pretty close to their chests, Dr Wilmott says the group has been proactive in quickly making all the information available to any other cancer researchers. ‘We’ve been doing this for a while, and the overarching goal is to put all this data together for researchers around the world to access,’ he says. ‘We’ve now made the whole genome sequences of 440 melanomas available to the international community, and the research community around the world can use it to find cures.’
By Ken Eastwood
Updated 4 years ago