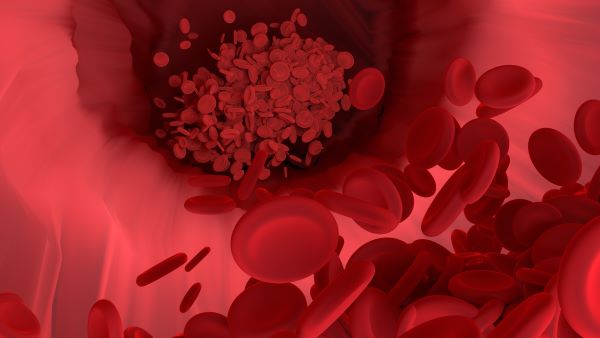
Blood-clot breakthrough paves the way for new drugs
“A better understanding of why clots form and why individuals can be resistant to the drugs developed to treat them will enable us to personalise therapy and develop more effective drugs.”
Professor Phil Hogg, Head of the ACRF Centenary Cancer Research Centre.

Millions of people are affected by blood clots each year – and a surprising new discovery about human blood-clotting proteins is paving the way for new treatment options.
Current anticoagulant drug treatments to prevent blood clots, also known as thrombi, are ineffective for about half of patients. This is a major problem, particularly for patients with heart disease or cancer, who die more often from blood clots.
The exciting discovery, that two human proteins involved in blood clotting and immunity exist in different and changing states, was made by Professor Philip Hogg, Head of the ACRF Centenary Cancer Research Centre, and his team.
According to Professor Hogg, this new knowledge about the form and function of clotting proteins could also shed light on why some people are more likely to form blood clots in the first place.
“But, importantly, it could show us why some people are often resistant to anticoagulant drugs and will enable us to personalise therapy and develop more effective drugs,” he says. “If you’re designing a drug based on the premise that disulphide bonds are formed the drug will not work for all people.”
Bond breakthrough
Proteins are the most sophisticated molecules made in nature, responsible for all of life’s processes. They consist of unique sequences of amino acids, and disulphide bonds link the amino acid chains together, like balls on a string.
From the early 1960s, when they were discovered, it was believed that these disulphide bonds were fully formed in the mature and functional protein, just keeping it stable and in its correct shape while it works.
However, Professor Hogg and his team found that the blood proteins they studied are being produced in multiple disulphide-bonded states.
“We were able to precisely measure whether the disulphide bonds in the blood proteins were formed or broken. What was surprising was that the bonds aren’t fully formed in the mature protein. They are made in multiple, possibly thousands, of different disulphide-bonded states,” he says. “What’s more, the unformed bonds are necessary for correct functioning of the protein.”
The long game
Professor Hogg’s discovery has been more than 20 years in the making and made possible with funding contributed by NSW Health’s Medical Research Support Program.
It stems from research he was conducting in 2000 when he was working with a human protein that was “doing something strange”.
“It contained a disulphide bond that, when cleaved by factors secreted by cells, changed how the protein worked – it bound to other proteins differently,” he says.
This observation led to Professor Hogg’s subsequent two decades of research on this biology.
“My team and I have been able to continue this research through grants and funding from the State and Federal governments. It is important to be able to pinpoint how drugs work in the setting of thrombosis,” he says.
Changing course
Professor Hogg believes their research will change how proteins are viewed and targeted in future drug and medical experiments.
“It’s starting to look like this is the norm,” he says. “It’s very likely that we will find many other proteins that exist in multiple states. Crucially, a drug may bind more or less preferentially to different states, impacting the effectiveness of the drug.
“In experimental settings, differing states of a protein should now be considered as part of the investigative medical research process.”
Updated 3 years ago